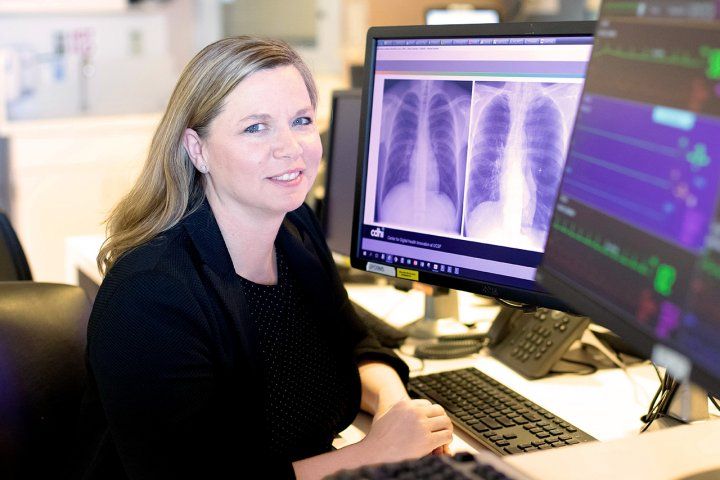
Trauma surgeon and data scientist Rachael Callcut explains how AI will transform our health.
By Ariel Bleicher UCSF Magazine
rachel-callcut-ai.jpg
The Future Visions for 2050
Artificial intelligence (AI) permeates our lives. It manages our phones and homes, helps us navigate, and advises us what to watch, read, listen to, and buy. Soon it will transform our health, says trauma surgeon and data-science expert Rachael Callcut, MD, MSPH. She answers some questions about the AI future:
What is the advantage of AI in medicine?
There is a certain amount of bias that we, as humans, bring to any clinical scenario: Without even realizing it, we may look past critical pieces of information that could help our patients get better. AI, which is essentially a computer algorithm that learns from data, can uncover patterns that we can’t see – either because of those biases or because the human brain simply can’t assimilate the vast quantity of medical data that is now available from hospital sensors and other digital health devices. Ultimately, AI promises to reduce human error and make our care more efficient, which will improve outcomes for our patients.
How is AI used in clinics today?
Its footprint is still relatively small. Only about 20 to 25 AI applications for health care have been cleared by the U.S. Food and Drug Administration. Most of these applications are marketed directly to consumers and are used for low-risk conditions – they do things like screen for eye disease or use your Apple Watch to detect certain heart-rhythm problems. Very few AI applications are actually used in hospitals for patient care, but this is beginning to change. For instance, my team at UCSF recently led the development of a new AI algorithm that works with portable X-ray machines. When a patient comes into an emergency room and gets a chest X-ray, the AI algorithm can review the image and detect certain life-threatening conditions, such as a collapsed lung. It can then alert the bedside clinician, which could lead to a faster diagnosis.
Imagine your wildest AI dreams have come true. A patient comes into the trauma bay. What happens next?
Data about the patient’s condition would already be streaming to us from emergency responders’ equipment. Then, as soon as the patient arrives at the hospital, we’d attach them to monitors. And as their vital signs are being tracked – and as physicians, surgeons, respiratory technicians, anesthesiologists, and everyone else is providing care and calling things out – an AI is recording all this information and integrating it into some kind of easy-to-navigate visualization on a screen.
Like in the film Minority Report?
Sure – we’re dreaming, right? You can imagine that very quickly we begin to see a story about the patient that could help us understand more rapidly what to do next.
What else is coming down the pike?
Within probably a decade, AI will be ubiquitous in the clinical environment. It will likely be embedded in ways that you, as a patient, may not even be aware of. As you are talking with your physician, for example, an AI application might be listening and crafting notes for your file. AI will certainly be an integral part of how we, as clinicians, take and read medical images. It will help us assimilate this information and other medical data to make informed recommendations, such as next steps or treatments that are optimal for your condition.
AI could also be used in your home and in consumer devices to learn your patterns: how many times you open the fridge, when you take your medications, how active you are – things like that. And if you’re not doing the same things you usually do, it could intervene and say, “That sounds like something you should call your doctor about.”
These are very far-fetched, “George Jetson” ideas. But it’s possible; the technology already exists.
Where will AI make the largest impact on health?
It may be in places around the world that do not have the resources of a big academic center like UCSF – a rural clinic, for example, or a battlefield, where a military corpsman is providing first-aid care. With AI, we can develop bedside tools and techniques that can help a less-experienced provider make more-informed clinical decisions.
It’s democratizing.
Absolutely. It’s leveling the playing field. AI has the capability, potentially, of exporting my knowledge as a trauma surgeon to places where I am not.
Most health professionals are women, but women make up only 35% of those with AI skills, according to the World Economic Forum. What’s at stake if we don’t close this gap?
I’m actually surprised that number is as high as it is because often I am the only woman at the table, which is unfortunate. The reality is that there are a lot of issues in women’s health that could be addressed with AI applications, but these tend not to be issues the field has focused on.
The other thing that happens – if you don’t have teams that are diverse – is we may be overlooking some nuances that are critically important for making these algorithms work for everyone. You have to have a diversity of backgrounds. You have to have people who consider that women’s bodies look different than men’s; that different populations may present with different symptoms; that they may have different preferences for how they interact with technology.
Will robots ever replace human doctors?
Never. If I told you, “You’re going to fly on a plane with no human pilot,” you’re not going to board that plane. It will be the same in medicine. AI is very powerful; it enhances what clinicians do and makes our jobs better. But we will always need to be there to guide it, inform it, and interpret what it’s doing.




